Introduction
New contraceptive options were supposed to bring huge improvements to “reproductive health.” Their proponents looked forward to a day when STIs and accidental pregnancies were a thing of the past.
It’s time to admit that hormonal birth control and condoms aren’t going to get us there.
Despite decades of innovation and availability of the “pill,” the “shot,” the IUD, and the “implant,” unwanted pregnancies are still common. Instead of enjoying “reproductive health,” women are suffering from a host of nasty side-effects. These methods even contribute to the abortion rate. (For more details, check out Human Life International’s free e-book on the contraception-abortion link.) And of course, hormonal contraception does nothing to protect users from disease.

But what about condoms? We’re told that we simply have to use a condom to ensure “safe sex.” Surely, handing out all that barrier-method birth control must have done something to contain the most problematic STIs, like HIV/AIDS.
Can you get an STD with a condom? If so, what are the odds of getting an STD with a condom?
The Centers for Disease Control (CDC) has reported that STIs are at all-time highs in recent years. For example, in 2008, about 25% of teenage girls had an STI. A decade later in 2018, estimates were about the same for adolescent females.
Total STI rates have reached record levels and are continuing to increase. Nearly half of the 26 million new STIs in America in 2018 affected 15-to-24-year-olds, according to the CDC.
Despite the fact that 43.9% of sexually active high schoolers used condoms as their primary contraceptives and 54.3% used one at their last sexual encounter in 2019, 1 in 4 teenagers get an STD every year.
So maybe it’s time to tell the truth: the “solution” was never a fix to begin with.
You Can Still Get STDs with Condoms
Condoms have been effectively marketed as an all-around “solution for those who want to embrace sexual activity without consequences. Many claim that condoms “protect” against pregnancy and STIs. But few stop to question whether condoms actually work. Those who think that condom usage will prevent any STIs are sadly mistaken. Let’s go point-by-point.

Even if a condom is used correctly and works perfectly, it is not effective at preventing exposure to infections that can be transmitted through skin-to-skin contact, or that affect areas not covered by the condom. Such infections include HPV, herpes, and syphilis. The condom’s ineffectiveness of protecting against such infections is admitted by several sources, including the CDC.1 All these STIs can have very serious negative health outcomes. Here are just a few examples:
- Genital warts are caused by human papillomavirus (HPV), the most common viral STD in the United States, accounting for three million new cases each year. HPV is present in an estimated 50% of all sexually active young women. As with other STDs, HPV is associated with multiple sexual partners and with earlier intercourse. As of 2018, about 43 million people were infected with it.
- Herpes genitalis is caused by the herpes simplex virus (HSV). Based on data, herpes infects 30 million+ people in the United States, most of whom show no symptoms. Those who do show symptoms may have painful ulcers in the genital or mouth area.2
- Syphilis, one of the deadliest STIs, recently reached historic highs, with 133,945 people in the United States newly infected in 2020. Untreated syphilis can lead to rashes, lesions, paralysis, aneurisms, blindness and even death.2
For STIs that should theoretically be kept under wraps by a condom, such as HIV, we need to look at condom failure rates to assess the risk factor.
Condom Failure Rates Are High
The oft-quoted statistic that condoms are 98% effective is misleading. The test that produced that data were conducted under laboratory conditions which do not accurately reflect the real world.
According to Contraceptive Technology, 21st Edition, the real-world success rate of condoms in preventing pregnancy is 87% over one year for couples who use condoms 100% of the time.3 What does that mean?

If condoms permit pregnancy among at least 13% of women using them in one year, then there is an even higher risk of HIV exposure, since not every condom “failure” or malfunction results in pregnancy (but each one does result in exposure to diseases spread through fluid exchange). The 13% failure rate over one year increases with time, reaching 50% at five years and 75% at 10 years. But all throughout that, the disease exposure rate is even higher.
Related: How Effective Are Condoms at Preventing Pregnancy?
Correct condom use is uncommon because it is complicated and involves significant attention to detail in moments when one is strongly distracted. A synthesis of 50 studies on condom use errors identified more than ten potential user errors, in addition to the issues of fit, slippage and breakage that are inherent to the condom itself. Several user errors were found to be extremely common, including failure to lubricate the condom (16.0% to 25.8% of participants), incorrect withdrawal (43% to 57% of condom use events), and incorrect storage (3.3% to 19.1% of participants). These error rates are recorded from populations in the USA, Canada, and the British Isles, where education about correct condom use is widely accessible.
In the third world, where information dissemination is limited by illiteracy, underdeveloped infrastructures, and lack of cultural awareness of condoms, these error rates are probably much higher. Even in the (highly unlikely) scenario that condom use errors could be globally eliminated, there is still the issue of condom failure, which was reported by 25% to 47% of participants surveyed.
According to a meta-analysis performed by HLI’s Dr. Brian Clowes, condoms either break or slip 6.06% of the time, which means there is an extremely high probability that a regular condom user will experience a catastrophic condom failure at some point, and with it the risk of exposure to any STI, including HIV.4
Chlamydia and gonorrhea are two of the most common STDs. While condoms decrease the risk of getting these STDs, their rates are still increasing.
- Chlamydia rates increased by 4.0% between 2020 and 2021. If left untreated, chlamydia can cause infertility, ectopic pregnancies, long-term pain, or blocked fallopian tubes in women.
- Gonorrhea rates increased 4.7% from 2020 to 2021. Left untreated, gonorrhea may at first be asymptomatic or may have milder symptoms. As times goes on, gonorrhea can cause pelvic inflammatory disease in women, which can lead to internal abscesses, infertility, and ectopic pregnancies. It can also spread to the blood, leading to disseminated gonococcal infection, which may be life-threatening.
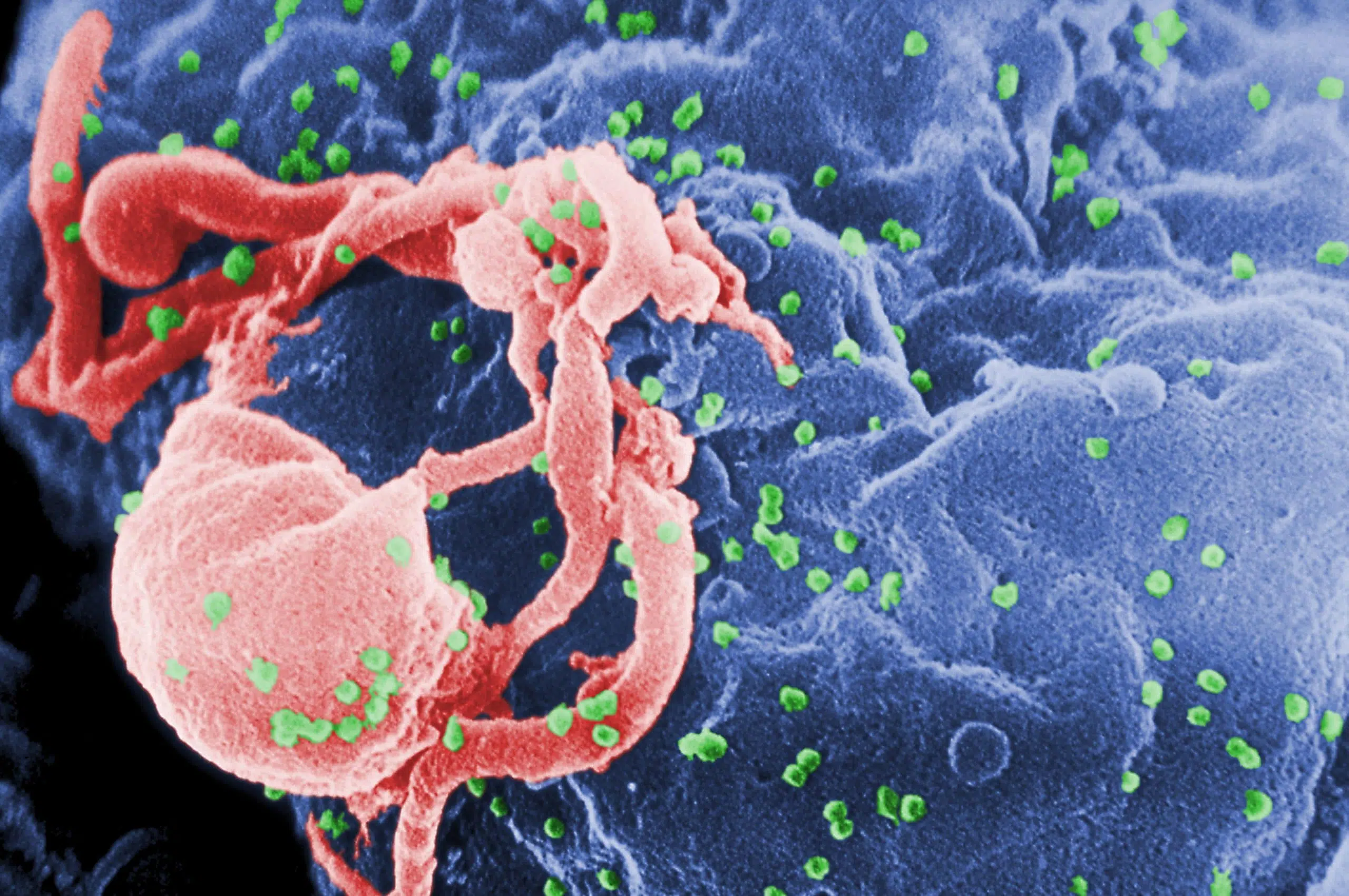
Condoms Are Ineffective Against HIV
According to the CDC, an unbroken and properly used condom is 99% effective at blocking HIV. These sound like excellent odds, until we consider:
- Condoms slip or break 6.06% of the time.
- Incorrect use is common.
- The integrity of a condom may be compromised before consumer purchase, especially in the third world, where manufacturing, shipping, and storage standards are lower.
- The studies found that 99% effectiveness did not simulate realistic conditions of intercourse.
Real-world analyses of condom efficacy in preventing HIV transmission are much less optimistic. One study showed, for example, that in monogamous, HIV serodiscordant male-female couples, only an 80% to 94% transmission risk reduction is granted. This sounds like a lot, but this means there is still at least 6% and up to 20% of the original risk of transmission (which is not given in the study). This risk increases cumulatively with each sexual act. Suddenly, condoms don’t sound very “safe.” One synthesis of studies focusing on heterosexual couples shows 80% protection per person-year, and another study shows 70% protection.
Related: Should the Church Let Serodiscordant Couples Use Condoms?
The outlook is no brighter for homosexual men engaging in receptive “sex” (sodomy) with HIV-positive partners. It is estimated that the lifetime risk of HIV for homosexual men is one in six.

Related: Is Homosexuality Really as Healthy as Heterosexuality?
Another analysis calculated the risk factor per sexual act and found that HIV is transmitted in 0.54% of acts unprotected by a condom and 0.20% of acts with condom protection. This translates to 63% prevention. The latest and most innovative analysis instead calculates condom effectiveness based on number of sexual partners, finding that for each partnership unprotected by a condom, there is an 83% chance of infection. Whereas, for partnerships that are always protected by condoms, the risk of infection is 7.3%, yielding a 91% condom effectiveness rate.
This relatively high protection rate is creating some excitement in the condom-promotion world, perhaps due to a general misunderstanding of what it actually means.
Infection rates rendered per act and per person-year compound, similarly to the pregnancy rates explained above. With every condom-protected act of this type, there is a 0.20% chance of infection. That sounds small, but with each additional act, there is again a 0.20% chance, which compounds to a significant risk for someone who engages frequently in sex (especially with multiple partners). There may be only a 3.8% chance of contracting HIV in one year, but who stops having sex after one year? The risk compounds year by year. At five years, you’ve reached a 17.6% chance of getting HIV.
The same is true of the per-partner analysis. There’s a 7.3% chance of infection with one sexual partner. But if the predominant practice were to have only one sexual partner, the AIDS epidemic would never have exploded. HIV infection compounds with every additional partner. That leads to a 20.3% infection rate after “only” three partners.
All this latest study has shown is that increasing the number of one’s sexual partners is as dangerous as we always knew it was, and that the solution is to live a monogamous lifestyle with a member of the opposite sex. This is because condoms do not eliminate the risk of HIV when used by those who engage in high-risk behaviors, such as promiscuity or sodomy. This is due to the fact that the cumulative probability of disease transmission increases significantly with each sexual act, and promiscuity and sodomy multiply risk by adding to the number of partners and involving contact with areas more prone to transmitting disease.
Condom Promotion Endangering the Third World
The disparity between the perception and reality of condom effectiveness has led to an unconscionable number of deaths, mostly in the third world, where government and health organizations have aggressively pushed universal condom use as a solution to the AIDS crisis.
Thailand
When the first HIV infections popped up in Thailand in 1991, the government enacted a “100% Condom Use Program.” This helped lead to an HIV infection rate of 9,072 per million 2003, according to the Joint United Nations Program on HIV/AIDS.4 In 2021, it had an adult (ages 15 to 49) HIV prevalence rate of 1%, or 1 in 100. A decrease in new HIV infections in the last decade is likely due mostly to anti-retrovirals.
The Philippines
The AIDS crisis reached the Philippines at the same time, but by 2003, that country had an infection rate of only 113 per million.5 As of 2021, the HIV prevalence rate remains a low 0.2% of adults 15-49, according to the Joint United Nation Program on HIV/AIDS (UNAIDS). Thailand’s infection rate is five times higher. The difference was the result of policy: in the Philippines, the government and the Church successfully encouraged young people to be abstinent before marriage and married people to remain faithful to their spouses.5
The success of this abstinence-based prevention program is much greater than what we see in the United States, where correct condom usage is an expected part of the high school health class curriculum. Despite all our “safe” sex education, first-world healthcare system and widespread condom availability, STI rates continue to increase among the youth.
About 1.2 million people have AIDS in the United States.
Countries that advocate “science” and “evidence” over “impractical” abstinence are suffering the consequences. Abstaining before marriage and faithfulness to one’s spouse are the best protections from STIs that exist.

Uganda
The abstinence approach also proved its effectiveness by reversing one of the worst HIV outbreaks in history. The ABC plan (Abstinence, Being faithful to one partner, Condoms if nothing else) cut the total HIV prevalence rate in Uganda from 15% in 1991 to 5% in 2001, the most positive trend in the world during that time.6
UNAIDS states that in 2018, there was a new infection rate of 1.4%. The total prevalence rate as of 2019 was 6.2%, including children born with AIDS, whereas of 2021, the adult prevalence rate is still only about 5.4%.7 All in all, for a country in a region that has struggled more with AIDS than any other parts of the world (including Southeast Asia), these numbers are phenomenal.
Condom promoters sometimes cite this information as an example of the success of condom-based responses to the AIDS crisis, but the reality is that the ABC program placed very little emphasis on condoms, and only promoted them for certain high-risk groups, such as prostitutes. Though it is debated whether the ABC effort’s success was based on abstinence and fidelity primarily or only partly, the fact of the matter is that the “A” and the “B” mattered a lot. Throughout the years of the ABC program, the average age of “sexual debut” increased among young men and women. But the average number of sexual partners decreased.8
Lesotho
Countries that emphasized condoms, however, had and still have the highest rates of infection.
One example is Lesotho, which had a condom usage rate of 40% among women 15-24 in 2019. This was the highest rate in the region. Despite this, Lesotho’s HIV prevalence among 15–49-year-olds in 2000 was 21.8%. After two decades, in 2022, it only marginally decreased to 19.3%.
Eswatini
Eswatini is another example. In 2010, Eswatini’s condom use rate was 44.7%.9 However, Eswatini also had the world’s highest HIV prevalence rate for a decade, despite roughly a 66% drop in new infections. In 2010, Eswatini’s HIV rate was 27.6%, and in 2020, the rate was 26.8%.10 Even so, the drop in HIV incidence was largely due to anti-retrovial therapy (ART). ART decreased the incidence of HIV between 2020 and 2016 by 43.57% among 15-49-year-olds.
Conclusions on Condom Promotion
In 2004, the journal Studies in Family Planning concluded, “No clear examples have emerged yet of a country that has turned back a generalized epidemic primarily by means of condom promotion.” This still holds true today. In fact, the primary reason why there has been a decline in AIDS transmission in Sub-Saharan Africa, from an estimated 2.2 million new infections (2005) to an estimated 670,000 (2021), is the expanded use of anti-retrovial technology, not condoms.11 Yet the United Nations, the European Union and its member countries, some U.S. agencies, and international organizations continue to promote condom use as the primary method of combating the spread of HIV and other STIs.
Rather, the key to success is in behavior change. According to a 2004 synthesis of the results of third-world AIDS prevention strategies, the main contributing factor reducing HIV infection rates among heterosexual couples was not condom use, but reduction in the number of sexual partners.12 For example, by 2000, the Ugandan Demographic and Health Survey found that 93% of Ugandans had changed their sexual behavior to avoid HIV/AIDS.
Contrary to all expectations, young Ugandans widely embraced the pro-abstinence message. From 1989 to 1995, the percentage of unmarried young men having sex plunged from 60% to 23%, and the percentage of unmarried young women having sex dropped from 53% to 16%.13 This proves that teenagers are not helpless slaves of their “raging hormones.” In South Africa, on the other hand, increases in condom availability were accompanied by increases in the number of persons who reported having more than one sexual partner.14 This is because condom promotion may lead to more risky behaviors by creating the illusion that sex with condoms is “safe.”
This illusion that a layer of latex removes all consequences from sexual activity is extremely dangerous. It’s dangerous, because condoms do not provide anything close to complete protection from HIV exposure.
Of course, condom promotion is only a symptom of the modern-day colonialism that plagues developing nations. The developed world – and especially the U.S. and the United Nations – insist on promoting abortion, family planning, sterilization, and acceptance of homosexuality in sovereign nations where their culture rejects such ideas. The developed world is determined to force its values and ideas onto developing countries, which can do little to stop it.
How to Actually Prevent STDs
The only acceptable prevention that is 100% effective is also Catholic-approved! Abstain from sexual activity before marriage, and if you marry, be faithful for life to your spouse.
Related: The Catholic Church on Contraception: An Introduction
You care about your physical welfare. The Catholic Church, knowing the science, isn’t trying to spoil your fun, but to teach the Truth. Respect yourself and your spouse if you have one, because everyone is made in the image and likeness of God. Sexual intimacy is not for selfish gratification, but rather it unifies husband and wife and invites the gift of children.
The human family is so beautiful that the only way to preserve it is to care for the soul as well as the body. We have many, many articles explaining why contraception is not only unhealthy, but also spiritually harmful. Remember, if there is no such thing in life as a free lunch, do you honestly believe sexual gratification would come without consequences?
If you are single, or in the religious life, please respect your own human dignity; live a life of chastity and abstinence. Many today buy into the secular lie that this is impossible. It’s not. Advocates for sexual “freedom” often forget that humans also have the freedom and the ability not to have sex. It’s a choice. No one “dies” of abstinence. Faithful Catholics have been engaging in abstinence or chaste behavior according to their state in life for millennia. And waiting for the right spouse is not only healthier physically, but it’s also spiritually beneficial to your soul.
Abstaining Until Marriage and Fidelity Are Beneficial for Your Health and Relationships
Being in a committed and monogamous relationship has multiple benefits, including an increase of trust, a reduced risk of STDs/STIs and the assurance that your partner will always be around. Plus, your children will grow up with both parents, which creates a stable environment for their development.
Saving sex for marriage also reaps many benefits. These benefits include being able to discern marriage without the emotional complications of a sexual relationship (or perhaps, having a child with that person) and dignifying sex as something exclusive, unique, and only to be shared within the lifelong covenant of marriage. This gives sex a deeper meaning than simple pleasure. It becomes something special that both partners are discovering together within the safety of marriage.
Read next: How Effective Are Condoms Against Pregnancy?
Dr. Brian Clowes’ research contributed to this report. This article was originally published in July 2022 by Jenna McGuire and was most recently updated in November 2023 by Marisa Cantu.
+ Endnotes
[1] “Syphilis – CDC Fact Sheet (Detailed),” Centers for Disease Control and Prevention; “Genital HPV Infection – Fact Sheet,” Centers for Disease Control and Prevention; “Genital Herpes – CDC Fact Sheet,” Centers for Disease Control and Prevention; Warner et al., “Condom Use and Risk of Gonorrhea and Chlamydia: A Systematic Review of Design and Measurement Factors Assessed in Epidemiologic Studies,” Sexually Transmitted Diseases 33, no. 1 (January 2006): 36-51.
[2] “Syphilis – CDC Fact Sheet (Detailed),” Centers for Disease Control and Prevention; “Genital HPV Infection – Fact Sheet,” Centers for Disease Control and Prevention; “Genital Herpes – CDC Fact Sheet,” Centers for Disease Control and Prevention; United States Department of Commerce, Bureau of the Census, Reference Data Book and Guide to Sources, Statistical Abstract of the United States 2012 (132nd Edition) (Washington, D.C.: United States Government Printing Office, 2012), Table 184, “Selected Notifiable Diseases – Cases Reported: 1980 to 2009.” “Herpes: HSV-1 and HSV-2.” Johns Hopkins Medicine. Accessed October 31, 2023. https://www.hopkinsmedicine.org/health/conditions-and-diseases/herpes-hsv1-and-hsv2.
[3] Hatcher, Robert, et al., Contraceptive Technology (21st Edition; New York: Ayer Company, 2018), 100.
[4] Trujillo, Alfonzo Cardinal Lopez, and Brian Clowes, The Case Against Condoms: The Scientific and Moral Basis for the Teaching of the Catholic Church on Preventing the Spread of Disease (Front Royal, Virginia: Human Life International, 2006).
[5] Ibid.
[6] Trujillo and Clowes, Case Against Condoms; Elaine M. Murphy et al., “Was the “ABC” Approach (Abstinence, Being Faithful, Using Condoms) Responsible for Uganda’s Decline in HIV?” PLOS Medicine 3, no. 9 (September 2006): e379.
[7] “12th Annual Joint AIDS Review (JAR) Final Report, July 2018 – June 2019: Empowering Young People to Champion the End of New HIV Infections,” Uganda AIDS Commission and UNAIDS, September 2019, 1; UNAIDS Data 2021, 90.
[8] Murphy et al., “Was the ‘ABC’ Approach Responsible?”
[9] “Condom Use, HIV Testing,” The Herald (Zimbabwe).
[10] UNAIDS Data 2021, UNAIDS, 64.
[11] Kharsany, Ayesha B. M., and Quarraisha A. Karim, “HIV Infection and AIDS in Sub-Saharan Africa: Current Status, Challenges and Opportunities,” Open AIDS Journal 10 (2016): 34-48.
Moyo, Enos, Perseverance Moyo, Grant Murewanhema, Malizgani Mhango, Itai Chitungo, and Tafadzwa Dzinamarira. “Key Populations and Sub-Saharan Africa’s HIV Response.” Frontiers in Public Health, May 16, 2023.
[12] Norman Hearst and Sanny Chen, “Condom promotion for AIDS prevention in the developing world: is it working?” Studies in Family Planning 35, no. 1 (2004).
[13] Joint United Nations Program on HIV/AIDS (UNAIDS), “Uganda: Epidemiological Fact Sheet on HIV/AIDS and Sexually Transmitted Diseases,” 2000.
[14] Zuma, Khangelani, et al., (2016). “New insights into HIV epidemic in South Africa: key findings from the National HIV Prevalence, Incidence and Behaviour Survey, 2012,” African Journal of AIDS Research 15, no. 1 (March 2016): 67-75.





Great work…